FALLBACK PLANNING
Fallback plans are generated after plan approval, based on previously created protocols.
If a machine is out of operation for any reason, fallback plans can be accessed and pushed via DicomRT to the R&V system.
BENEFITS
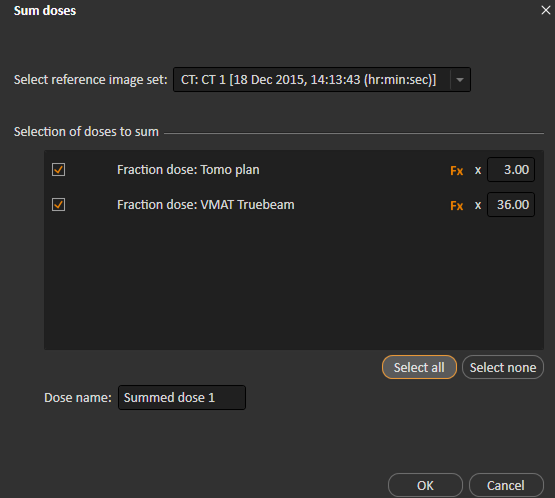
1. Avoid treatment disruptions. Create a contingency plan that is saved until needed, such as in the event of machine outage. The fallback plan can then be pushed to the machine for delivery. RayStation also has powerful tools in plan evaluation, which allow the user to combine treatments performed on different machines, e.g., it is possible to combine 27 fractions using a Tomotherapy machine with 3 fractions using a conventional linac and view the resulting total dose.
2. Compare efficacy of different treatment techniques.
a. For instances where reimbursement requirements state that the most suitable treatment plan must be utilized, fallback planning eliminates the need for an extra plan to be submitted for billing purposes.
3. Can convert between different modalities and treatment techniques, e.g. can be used to convert proton or tomotherapy plans to VMAT, IMRT or 3D-CRT.
DOSE MIMICKING ALGORITHM
Fallback plans are generated by a dose mimicking optimization that seeks to recreate or improve the dose distribution of the initial plan. The optimization penalizes dose differences relative to the initial plan both on a voxel-per-voxel level and in terms of DVH curves. Dose for OARs is only penalized if it exceeds the dose of the original plan whereas dose for targets is penalized if uniformity has deteroriated compared to original plan. The result of the dose mimicking optimization can be customized with user-specified parameters such as:
• The priority between minimization of voxel-wise dose differences and DVH curve differences
• The priority between target uniformity and sparing of OARs
• Which regions of interest that the mimicking should consider
CREATING A FALLBACK PLAN
The first step in utilizing the Fallback module is to create the desired protocols. This is a simple process that allows customization to the specific machines in use at the clinic, and defines the types of plans to “fall back” to. At the completion of any treatment plan, the fallback plans can be automatically created and will remain stored in the system until needed.
If a machine failure occurs, or a patient requires repositioning, the replanning process is already complete and the fallback plan is ready to use. New plans are housed in a separate location called ”fallback plans”. The clinical goals of the initial plan are moved over to the fallback plans, allowing the user to see if the new plan meets planning objectives. It is important to note that if additional optimization is required on the fallback plan, it is possible to do so.
When the use of a fallback plan becomes necessary, the user will access the saved fallback plans, evaluate which one is most suitable, and copy it to the plan list. It is then possible to select which fraction the plan will begin at. Going forward, the plan remains in the plan list, with flexibility to modify as needed. The selected plan requires approval before it can be sent to the machine for treatment.
Once the patient is able to return to the originally planned machine, there is an option in the fallback module to “return to original plan”. It is also possible to sum the dose in plan evaluation by defining the fractions used with each treatment modality or machine.